Introduction To
Understanding Back Pain: A Four-Bucket Approach for Long Island & Nassau County Patients
At Mosaic Pain Medicine & Rehabilitation in Cedarhurst, NY—serving patients throughout Nassau County and the Five Towns of Long Island—we believe that the first step toward lasting back-pain relief is education. Research shows that up to 84 percent of adults will experience back pain during their lifetime, and while most acute episodes of back pain subside within 12 weeks, chronic lower-back pain can dramatically limit work, family life, and recreation if left untreated.
To help our Long Island neighbors understand what’s happening inside their bodies, Dr. Brian Singer teaches every patient a simple, four-bucket model of spinal anatomy and pain generators:
- Bones
- Nerves
- Muscles
- Tissues
By pinpointing which “bucket” is driving your discomfort, we can pair targeted therapies such as epidural steroid injections, trigger-point injections, or radiofrequency ablation with a personalized rehabilitation plan.

Bones of the Spine (Vertebrae)
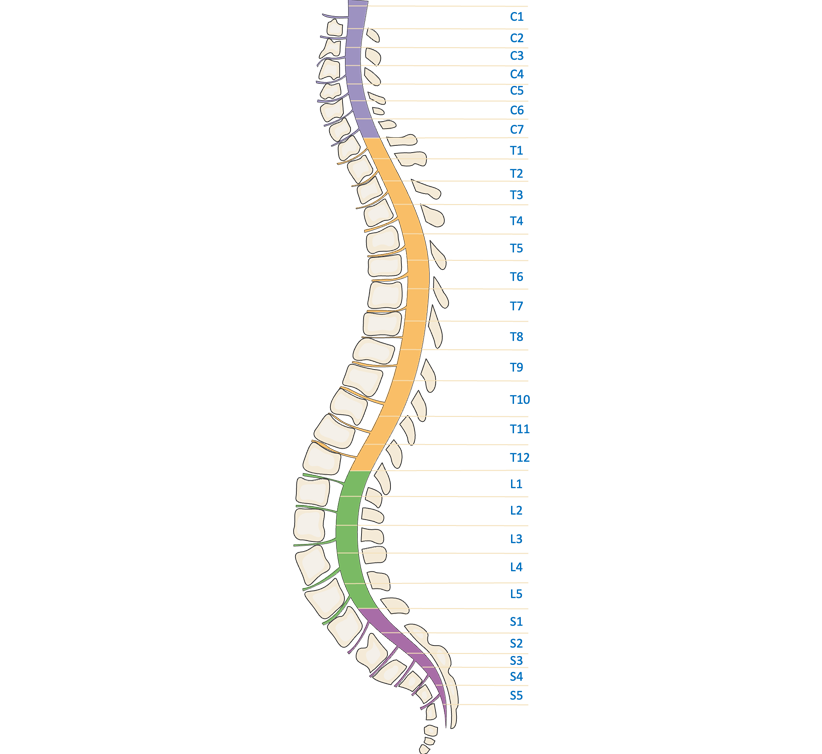
- Cervical Spine (Neck) – These support the head and allow for movements like nodding and turning.
- Thoracic Spine (Mid-Back) – These vertebrae are unique that they are attached to the ribs
- Lumbar Spine (Lower Back) – There are five vertebrae (L1-L5) in this region and are the largest and bear most of the body’s weight. These are the most affected bones that cause most of the back pain.
- Sacrum and Coccyx (Pelvic Area) – The sacrum consists of five fused vertebrae (S1-S5) that connect the spine to the pelvis, while the coccyx (tailbone) is made of three to five fused bones, providing support when sitting.
Nerves of the Spine (Spinal Cord and Peripheral Nerves)
- Cervical Nerves (C1-C8) – Control movement and sensation in the head, neck, shoulders, arms, and hands.
- Thoracic Nerves (T1-T12) – Control the chest and upper abdominal muscles.
- Lumbar Nerves (L1-L5) – Control the lower abdomen, legs, and parts of the feet.
- Sacral Nerves (S1-S5) – Affect the hips, buttocks, legs, and bladder control.
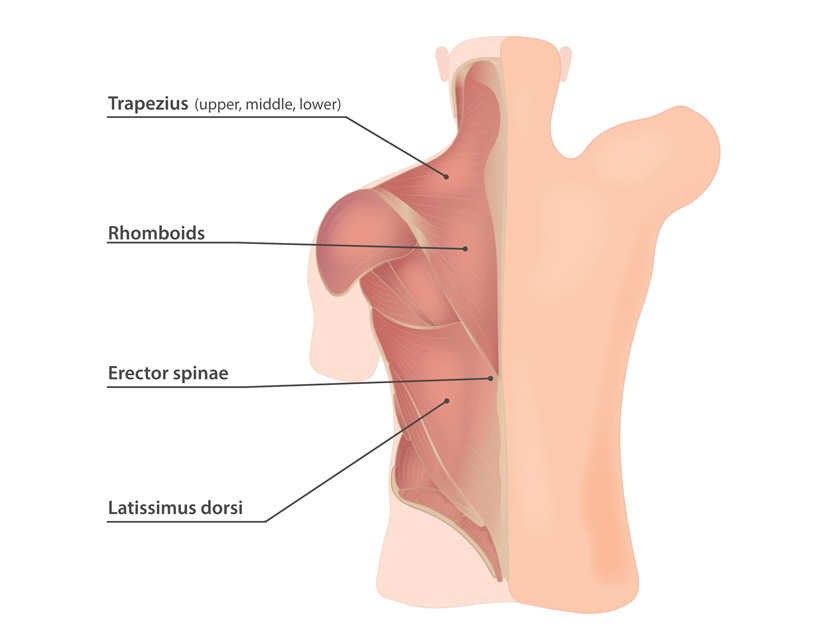
Muscles of the Spine
- Deep Muscles – These help with posture and stabilization and include the paraspinals, erector spinae and multifidus.
- Superficial Muscles – These include the trapezius, latissimus dorsi, and rhomboids.
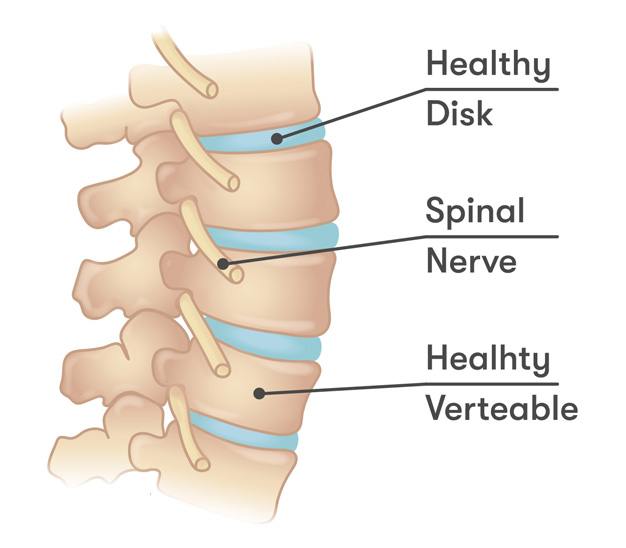
Tissues of the Spine (Discs, Ligaments, and Cartilage)
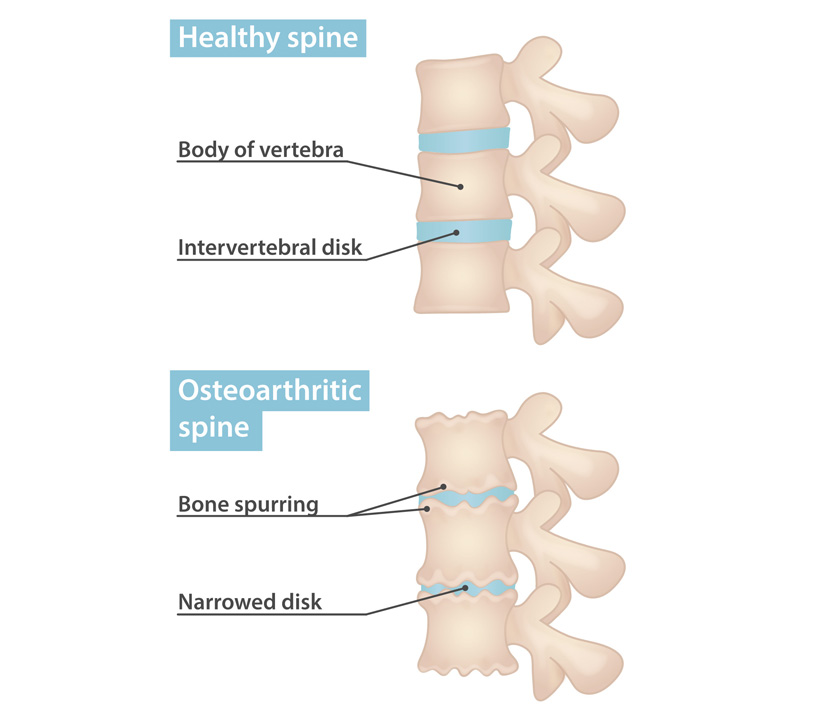
- Intervertebral Discs – These cartilage cushions sit between the vertebrae, absorbing shock and preventing bone-on-bone contact. Each disc has a tough outer layer (annulus fibrosus) and a gel-like inner core (nucleus pulposus).
- Ligaments – These tough bands hold the vertebrae together and maintain spinal stability. Two major structures include anterior longitudinal ligament (which prevents excessive backward bending) and the posterior longitudinal ligament (which limits forward bending).
- Cartilage and Facet Joints – Cartilage lines the small facet joints, allowing smooth movement between vertebrae while preventing excessive twisting or bending.
Our Treatment Approach
-

Comprehensive Lifestyle
Lifestyle Modification Combined with patient tailored cognitive behavioral therapy referral, nutrition, vitamin supplementation
-

Physical and Occupational Therapy
Physical and Occupational Therapy for Functional Improvement
-

Non-Opioid Medication Management
Medications non opioids oral medications
-

Targeted Injections for Pain Relief
Injections; targeting muscle, nerve, bone or sympathetic
-

Neuromodulation Techniques for Pain Management
Neuromodulation; spinal cord stimulation, dorsal root ganglion stimulation, peripheral nerve stimulation
-

Specialist Referrals for Advanced Care
Referral to my colleagues specialized in orthopedic surgery, neurosurgery or neuropsychology.
