Introduction To
Knee Anatomy for Pain Management
Knee pain is one of the most common chronic pain complaints I get in my office. The first step to tackling knee pain whether it’s just started it or it has been going on for years is to understand the complex structure of the knee. Our knees are a joint that bear nearly all the body weight and play a critical role in movement and stability. Understanding the knee anatomy is crucial for patients managing knee pain and I like to break it up into 4 different buckets:
- Bones
- Nerves
- Muscles
- Connective tissues
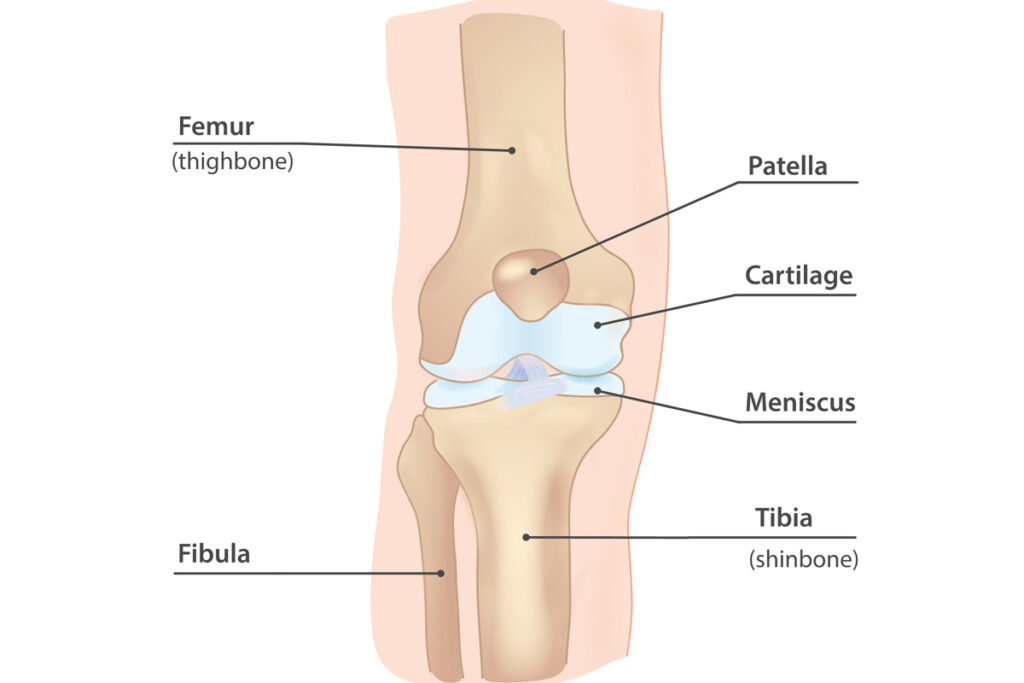
Bones
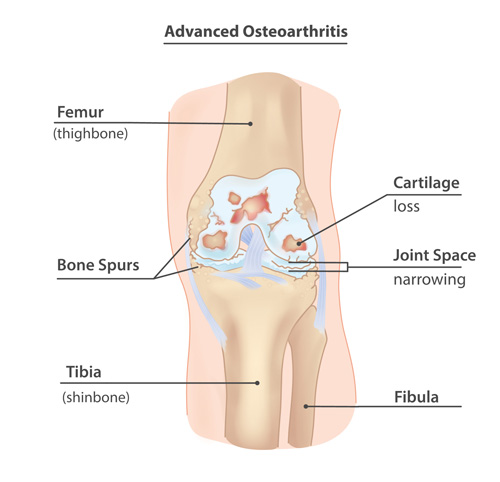
The knee’s bony structure consists of three primary bones
- Femur (Thigh Bone): The largest bone in the body that forms the upper portion of the knee joint.
- Tibia (Shin Bone): The primary weight-bearing bone of the lower leg that articulates with the femur.
- Patella (Kneecap): A protective bone that enhances leverage for the quadriceps muscle.
Key joint structures formed by the connection of any two bones of thn knee include the medial tibiofemoral joint, lateral tibiofemoral joint, and patellofemoral joint, which are common sources of arthritis, injury, or instability.
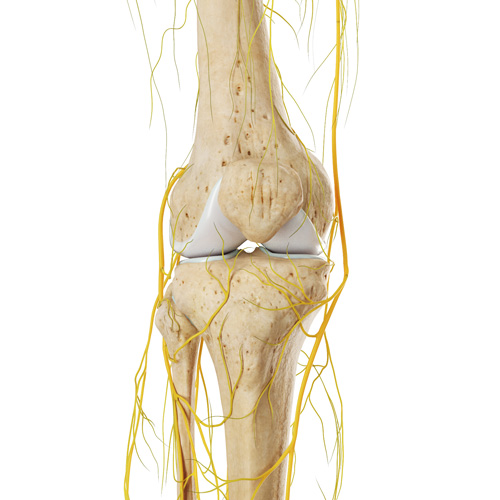
Nerves
The knee’s nerve supply is critical for movement and sensation. Key nerves influencing knee function include:
- Femoral Nerve: Controls the quadriceps and supplies sensation to the anterior thigh and knee.
- Sciatic Nerve: Branches into the tibial and common peroneal nerves, which influence knee flexion and calf muscle control.
- Saphenous Nerve: A branch of the femoral nerve that provides sensation to the inner knee and calf.
- Peroneal Nerve: Wraps around the fibula and is vulnerable to injury; compression can cause weakness and foot drop.
- Genicular nerves: Nerve endings supplying sensation to the knee.
Nerve entrapments, compression syndromes, or neuropathy can contribute to knee pain, requiring careful diagnosis and treatment.
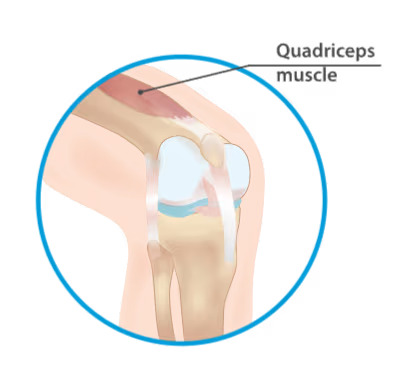
Muscles
The shoulder’s muscle groups provide stability, control, and movement. Key muscles relevant to pain management include:
- Muscles of the front of the thigh include the Quadriceps (Rectus Femoris, Vastus Medialis, Vastus Intermedius, Vastus Lateralis): Extend the knee and are ripe to overuse or strain injuries.
- Muscles of the back of the thigh include the Hamstrings (Biceps Femoris, Semitendinosus, Semimembranosus): Control knee flexion and stabilize the joint.
- Muscles of the calf include the Gastrocnemius and Soleus: Support knee flexion and ankle movement; tightness can impact knee function.
Muscle imbalances, strains, and weakness are common contributors to knee pain and are often treated with strengthening exercises, stretching, and skilled physical therapy.
Connecting Tissues
Connective tissues in the knee play a crucial role in stability and cushioning.
- Menisci (Medial and Lateral): C-shaped cartilage that cushions the knee joint; tears are a common cause of pain and dysfunction.
- ACL and PCL (Crucial ligaments): Provide anterior and posterior knee stability; ACL injuries are common in sports and affected athletes like Tom Brady and Derrick Rose.
- Collateral Ligaments (MCL and LCL): Stabilize the knee from side-to-side forces.
- Patellar Tendon: Connects the patella to the tibia and can become inflamed in conditions like patellar tendonitis.
- Bursae: Fluid-filled sacs that reduce friction and cushion the knee joint. Key bursae in the knee include:
- Prepatellar Bursa: Located in front of the patella, this bursa often becomes inflamed in conditions like "housemaid's knee."
- Infrapatellar Bursa: Found below the patella, this bursa reduces friction between the patellar tendon and the tibia.
- Suprapatellar Bursa: Positioned above the patella, inflammation here may mimic knee joint pain.
- Pes Anserine Bursa: Located on the inner knee below the joint, inflammation here can cause medial knee pain, especially in athletes or patients with osteoarthritis.
Our Treatment Approach
At Mosaic Pain and Medicine Rehabilitation, we take a multidisciplinary approach to back pain treatment, combining diagnostic expertise, interventional pain procedures, and rehabilitation strategies to provide lasting relief.
-

Comprehensive Lifestyle
Lifestyle Modification Combined with patient tailored cognitive behavioral therapy referral, nutrition, vitamin supplementation
-

Physical and Occupational Therapy
Physical and Occupational Therapy for Functional Improvement
-

Non-Opioid Medication Management
Medications non opioids oral medications
-

Targeted Injections for Pain Relief
Injections; targeting muscle, nerve, bone or sympathetic
-

Neuromodulation Techniques for Pain Management
Neuromodulation; spinal cord stimulation, dorsal root ganglion stimulation, peripheral nerve stimulation
-

Specialist Referrals for Advanced Care
Referral to my colleagues specialized in orthopedic surgery, neurosurgery or neuropsychology.
General Questions
Knee pain can result from arthritis, ligament injuries (ACL, MCL), meniscus tears, tendonitis, bursitis, or cartilage degeneration due to aging, overuse, or injury.
We offer physical therapy, knee injections (such as corticosteroid and hyaluronic acid injections), radiofrequency ablation, platelet-rich plasma (PRP) therapy, and other non-invasive treatments to relieve pain and improve mobility.
You should seek medical attention if your knee pain persists for more than a few weeks, worsens over time, limits mobility, or is accompanied by swelling, instability, or clicking sounds.
Yes, most knee conditions can be managed with non-surgical treatments, including physical therapy, medications, injections, and minimally invasive procedures like radiofrequency ablation or nerve stimulation. Surgery is considered only for severe cases.
Share this page:
Facebook
LinkedIn
Twitter
