Introduction To
Neck Anatomy for Pain Management
It is important to recognize and appreciate that the neck is the structure holding our head/brain to our body. All motor commands from the brain must travel down through the neck and all sensory input from the body must travel up through the neck. The neck houses crucial anatomical components like our spinal cord that support movement, provide stability, and facilitate essential functions like breathing and circulation. Understanding these structures is important for patients managing neck pain, as many pain-related issues stem from dysfunction or injury to these anatomical features. Below I have broken up the elements of the neck into four major buckets including:
- Bones
- Nerves
- Muscles
- Tissues


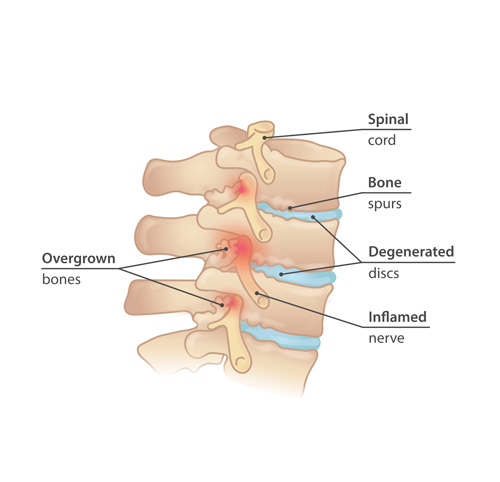
Bones
The skeletal structure of the neck is formed by the cervical spine, consisting of seven vertebrae (C1 to C7). Each vertebra plays a distinct role and can be a source of neck pain if injured or degenerated:
- C1 (Atlas): Supports the skull and enables nodding motion. Misalignment here can cause headaches and upper neck pain.
- C2 (Axis): Features the odontoid process (dens) that facilitates rotational movement. Injuries to this area may cause restricted rotation and radiating pain.
- C3 to C7: Typical cervical vertebrae with bifid spinous processes and transverse foramina for blood vessels. These are common sites for degenerative changes such as arthritis and disc herniation, which can lead to nerve impingement.
Conditions like cervical spondylosis, fractures, and facet joint arthritis can significantly impact these structures, causing chronic pain.
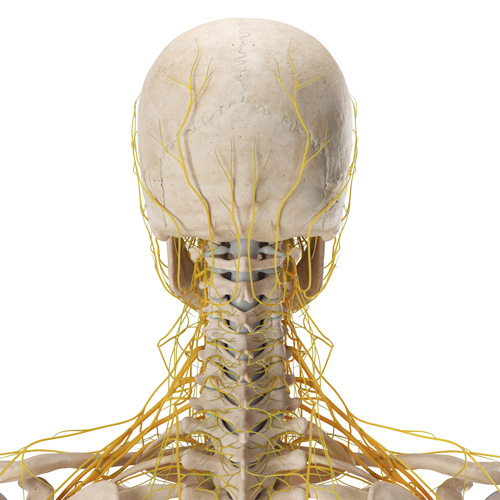
Nerves
The neck’s nervous system is intricate, containing both motor and sensory pathways that are key to understanding neck pain:
- Cervical Plexus (C1-C4): Supplies sensory and motor functions to the neck, scalp, and shoulders. Entrapment or irritation of these nerves can cause localized or referred pain.
- Brachial Plexus (C5-T1): Extends into the upper limbs for motor control and sensation. Compression in this region may cause symptoms such as numbness, tingling, or weakness in the arms.
- Vagus Nerve (Cranial Nerve X): Regulates parasympathetic functions in the thoracic and abdominal organs, which may contribute to headaches and neck tension.
Nerve impingement, radiculopathy, and neuropathic pain are common complaints in pain management and are often linked to cervical nerve dysfunction.
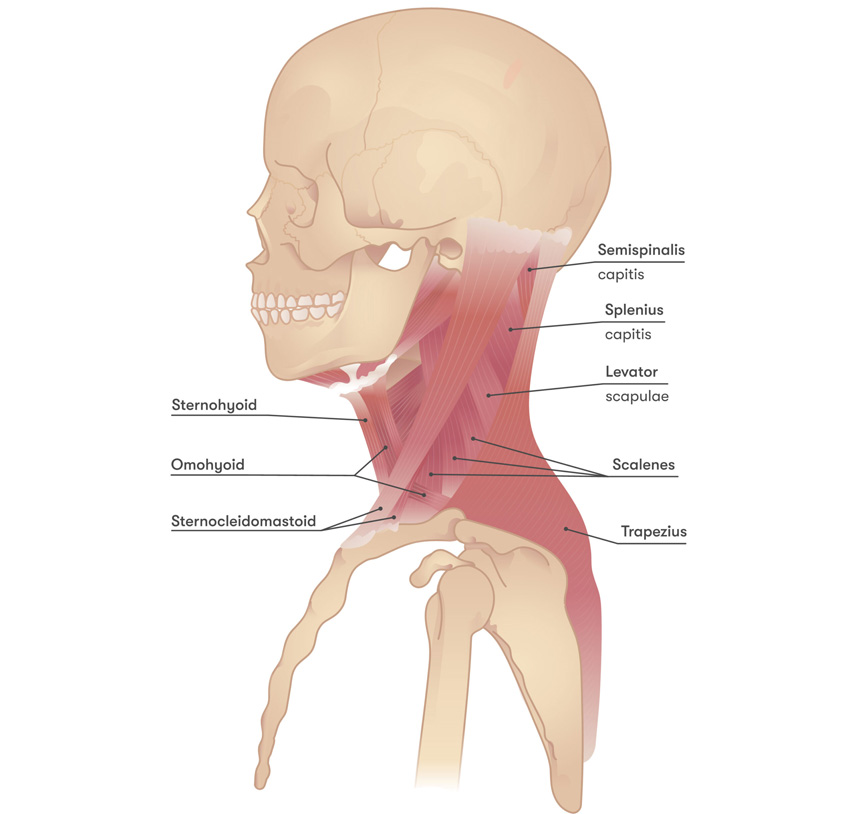
Muscles
The neck muscles enable motion, support posture, and protect underlying structures. Muscle strain and spasm are major contributors to neck pain. Major muscle groups include:
- Sternocleidomastoid (SCM): Aids in head rotation and flexion. Tension here can cause headaches, dizziness, and referred pain.
- Trapezius: Elevates and stabilizes the shoulder girdle. Trigger points in this muscle often contribute to tension headaches and upper back pain.
- Scalene Muscles: Assist in neck flexion and elevate the ribs during respiration. Tightness here can compress nerves, contributing to thoracic outlet syndrome.
- Levator Scapulae: Elevates the scapula and stabilizes neck movement. Dysfunction can cause neck stiffness and upper back pain.
- Deep Muscles (e.g., Cervical paraspinal muscles, Longus Colli, Longus Capitis): Provide fine motor control and cervical spine stabilization. Weakness or imbalance can contribute to chronic neck instability and discomfort.
Muscle imbalances, poor posture, and trigger points are common targets in pain management strategies.
Tissues
The neck contains various connective tissues that provide support, flexibility, and protection. Understanding these tissues is key to identifying sources of neck pain:
- Intervertebral Discs: These cartilage cushions sit between the vertebrae, absorbing shock and preventing bone-on-bone contact. Each disc has a tough outer layer (annulus fibrosus) and a gel-like inner core (nucleus pulposus).
- Ligaments: Such as the anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL), which stabilize the cervical spine. Ligament sprains are common in whiplash injuries.
- Fascia: Layers of connective tissue that compartmentalize muscles, nerves, and blood vessels. Tight or restricted fascia can cause referred pain and limit movement.
- Cartilage: Present in structures like the larynx and trachea, aiding in respiration and vocalization. Degenerative changes in cartilage may contribute to stiffness and discomfort.
- Blood Vessels: Including the carotid arteries and jugular veins, which are essential for blood supply to and from the brain. Circulatory issues can sometimes mimic neck pain symptoms.
Conditions like cervical disc herniation, DISH disease, and facet joint arthritis can significantly impact these structures, causing chronic pain.
Our Treatment Approach
At Mosaic Pain and Medicine Rehabilitation, we take a multidisciplinary approach to back pain treatment, combining diagnostic expertise, interventional pain procedures, and rehabilitation strategies to provide lasting relief.
-

Comprehensive Lifestyle
Lifestyle Modification Combined with patient tailored cognitive behavioral therapy referral, nutrition, vitamin supplementation
-

Physical and Occupational Therapy
Physical and Occupational Therapy for Functional Improvement
-

Non-Opioid Medication Management
Medications non opioids oral medications
-

Targeted Injections for Pain Relief
Injections; targeting muscle, nerve, bone or sympathetic
-

Neuromodulation Techniques for Pain Management
Neuromodulation; spinal cord stimulation, dorsal root ganglion stimulation, peripheral nerve stimulation
-

Specialist Referrals for Advanced Care
Referral to my colleagues specialized in orthopedic surgery, neurosurgery or neuropsychology.
General Questions
Chronic neck pain can result from poor posture, muscle strain, arthritis, herniated discs, nerve compression, or underlying medical conditions like spinal stenosis or degenerative disc disease. Our neck specialists will perform a thorough history and physical to pinpoint your cause of pain.
We offer a range of treatments, including physical therapy, injections (such as epidural and facet joint blocks), radiofrequency ablation, neuromodulation, neck massage, and non-invasive therapies like TENS and biofeedback.
You should seek medical attention if your neck pain persists for more than a few weeks, worsens over time, or is accompanied by numbness, weakness, or headaches. Early evaluation can help prevent long-term complications.
Yes, most cases of neck pain can be effectively managed with non-surgical treatments, such as physical therapy, medication, injections, and minimally invasive procedures like radiofrequency ablation and nerve stimulation. Surgery is only considered for severe cases.
Share this page:
Facebook
LinkedIn
Twitter
